In North Carolina, excessive alcohol use is the third leading preventable cause of death. With excessive alcohol consumption comes the risk of addiction – and when trying to stop drinking, withdrawal symptoms can set in. Sometimes, these symptoms can be overwhelming and require the help of professionals to overcome them. Because alcohol withdrawal can be a challenging and potentially dangerous process, medical intervention is often required to manage the withdrawal symptoms and prevent any complications. One medication often used to treat alcohol withdrawal is a benzodiazepine called Xanax.
Yes, Xanax may be used to manage the symptoms of alcohol withdrawal.
What is Alcohol Withdrawal?
Alcohol withdrawal occurs when an individual who has been consuming alcohol heavily and regularly suddenly reduces or stops their intake. This happens because the body, which has become accustomed to the depressive effects of alcohol on the central nervous system, reacts by overcompensating once alcohol is removed. As a result, a series of physical and psychological symptoms manifest, ranging from mild to severe.
Mild Symptoms
- Anxiety: Feelings of nervousness and worry.
- Tremors: Shaking, especially in the hands.
- Sweating: Increased perspiration, even without physical exertion.
- Nausea and Vomiting: Gastrointestinal distress, leading to nausea and sometimes vomiting.
- Headache: Persistent and often intense headaches.
- Insomnia: Difficulty falling or staying asleep.
- Loss of Appetite: Reduced desire to eat.
Moderate Symptoms
- Increased Heart Rate: Palpitations and a faster-than-normal heart rate.
- Elevated Blood Pressure: Higher blood pressure levels.
- Fever: Elevated body temperature.
- Mental Confusion: Difficulty concentrating or thinking clearly.
- Mood Swings: Rapid changes in mood, including irritability and depression.
Severe Symptoms
- Seizures: Convulsions that can be life-threatening.
- Hallucinations: Seeing, hearing, or feeling things that are not present.
- Delirium Tremens (DTs): A severe form of withdrawal that includes confusion, rapid heartbeat, high blood pressure, fever, and hallucinations. DTs can be fatal without medical treatment.
- Severe Agitation: Extreme restlessness and agitation.
- Disorientation: Loss of sense of time, place, or personal identity.
Alcohol Use Disorder Contributes to Alcohol Withdrawal
Alcohol Use Disorder (AUD) is a chronic condition characterized by an inability to control or stop drinking despite adverse social, occupational, or health consequences. It encompasses a range of behaviors and physical symptoms that signify a problematic relationship with alcohol. People with AUD may find themselves consuming more alcohol over longer periods than intended, experiencing strong cravings, and spending significant time obtaining, using, or recovering from alcohol.
People with AUD often face difficulties in fulfilling major responsibilities at work, school, or home due to drinking. The disorder can lead to tolerance (needing more alcohol to achieve the same effect) and withdrawal symptoms when alcohol use is reduced or stopped. AUD is a serious condition that requires professional treatment, which can include behavioral therapies, medication, and support groups to help individuals achieve and maintain sobriety.
Statistics on AUD in the United States
According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), in 2019, approximately 14.5 million people aged 12 and older had AUD. Among adolescents aged 12-17, around 414,000 had AUD, with the condition impacting 163,000 females and 251,000 males. The prevalence of AUD also varies across different racial and ethnic groups, with the highest rates observed in Native Americans and Alaska Natives.
AUD is more common among adults aged 18-29, with about 10.4% of this age group affected, compared to 4.7% of adults aged 30-44.

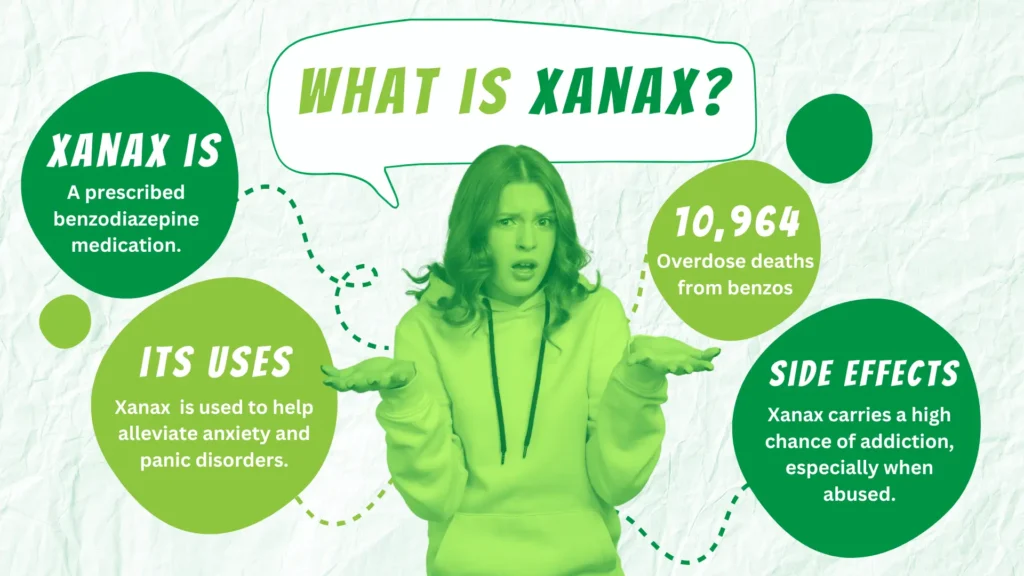
What is Xanax?
Xanax, also known as alprazolam, is a medication belonging to the benzodiazepine class. These medications are widely prescribed to treat anxiety and panic disorders. It works by enhancing the effects of gamma-aminobutyric acid (GABA), a neurotransmitter in the brain that promotes calmness and reduces nerve activity. Because of this, Xanax produces a calming effect, helping to alleviate symptoms of anxiety and panic such as excessive worry, agitation, and physical symptoms like muscle tension. Even though Xanax is effective, it carries a risk of dependence and abuse, particularly when used over an extended period or in higher doses than prescribed. For this reason, it is generally prescribed for short-term use and under careful medical supervision to minimize potential risks.
In 2022, the number of overdose deaths in the United States involving benzodiazepines totaled 10,964.
How Xanax is Used for Alcohol Withdrawal
Managing alcohol withdrawal can be a complex and challenging process, requiring medical intervention to ensure patient safety and comfort. Xanax can be used in the management of alcohol withdrawal symptoms, though it is not the most commonly prescribed medication for this purpose. The most important thing is understanding how Xanax can help, how to use it safely, and how to avoid addiction potential.
The Role of Benzodiazepines in Alcohol Withdrawal
Benzodiazepines are often employed in the treatment of alcohol withdrawal due to their calming effect on the central nervous system. This makes benzodiazepines particularly effective in managing the acute phase of alcohol withdrawal.
While Xanax can be effective, longer-acting benzodiazepines like diazepam (Valium) or chlordiazepoxide (Librium) are typically preferred in the treatment of alcohol withdrawal. These medications have a longer half-life, providing more prolonged coverage and a smoother tapering process, which helps prevent the recurrence of withdrawal symptoms. Xanax, with its shorter half-life, may require more frequent dosing and careful monitoring to avoid rebound symptoms.
Dosing and Administration
When Xanax is used for alcohol withdrawal, it is usually part of a comprehensive treatment plan that includes medical supervision and supportive care. The dosage is tailored to the individual’s specific needs, severity of withdrawal symptoms, and overall health status. The goal is to use the lowest effective dose for the shortest duration necessary to manage symptoms and prevent complications.
Risks and Considerations
Using Xanax for alcohol withdrawal carries certain risks, particularly the potential for dependence and abuse. Individuals with a history of substance abuse may be at higher risk of developing a dependency on Xanax, complicating their recovery process. Therefore, its use is carefully monitored by healthcare professionals, who may opt for alternative medications or treatment strategies based on the patient’s history and risk factors.
What To Expect During Alcohol Withdrawal Treatment
Treating alcohol withdrawal involves a comprehensive approach designed to alleviate symptoms, prevent complications, and provide support through the detoxification process. The severity of alcohol withdrawal can vary significantly, so treatment plans are tailored to the individual’s needs and may take place in various settings, from outpatient clinics to inpatient hospitals or specialized detox centers.
Initial Assessment
The first step in treating alcohol withdrawal is a thorough medical assessment. Healthcare professionals evaluate the patient’s drinking history, the severity of withdrawal symptoms, overall health status, and any co-occurring mental health conditions or substance use disorders. Tools like the Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) may be used to gauge symptom severity and guide treatment decisions.
Medical Supervision and Monitoring
Due to the potential for severe complications, medical supervision is critical during alcohol withdrawal. Patients are monitored for vital signs, hydration status, and symptom progression. In severe cases, continuous monitoring in an intensive care unit (ICU) may be necessary.
Medications are a cornerstone of alcohol withdrawal treatment, aimed at reducing symptoms and preventing complications:
- Benzodiazepines: Medications such as Xanax, diazepam (Valium), chlordiazepoxide (Librium), and lorazepam (Ativan) are commonly used to manage anxiety, agitation, and seizures. These drugs mimic the effects of alcohol on the brain, helping to stabilize the central nervous system.
- Anticonvulsants: These may be used to prevent or treat seizures in patients who do not respond adequately to benzodiazepines.
- Beta-Blockers and Alpha-Agonists: Medications like propranolol or clonidine can help manage autonomic symptoms such as high blood pressure and rapid heart rate.
- Vitamins and Electrolytes: Thiamine (vitamin B1) is often administered to prevent Wernicke-Korsakoff syndrome, a severe neurological condition associated with chronic alcohol abuse. Other vitamins and electrolyte supplements may be given to address deficiencies.

Supportive Care
Supportive care is vital to ensure the patient’s comfort and well-being during withdrawal:
- Hydration: Maintaining adequate fluid intake is crucial, as dehydration is common during alcohol withdrawal.
- Nutritional Support: Proper nutrition helps in recovery and addresses any deficiencies caused by chronic alcohol use.
- Rest and Sleep: Creating a calm, quiet environment can aid in reducing agitation and promoting restful sleep.
Psychological and Emotional Support
Alcohol withdrawal can be a distressing experience, making psychological and emotional support essential. Short-term counseling or therapy helps individuals cope with the emotional challenges of withdrawal, providing professional guidance and strategies for managing stress and anxiety. Participation in support groups, such as Alcoholics Anonymous (AA), offers ongoing emotional support and encouragement from others who have faced similar struggles, fostering a sense of community and shared experience that can be crucial for recovery.
Find an AA meeting near you in North Carolina – https://aanorthcarolina.org/.
Long-Term Treatment and Follow-Up
Successfully managing alcohol withdrawal is only the first step in addressing alcohol use disorder. Long-term treatment and follow-up care are crucial to maintaining sobriety and preventing relapse:
- Rehabilitation Programs: Inpatient or outpatient rehabilitation programs offer comprehensive treatment, including counseling, therapy, and education about addiction.
- Medication-Assisted Treatment (MAT): Medications such as naltrexone, acamprosate, or disulfiram may be prescribed to help reduce cravings and support long-term abstinence.
- Continued Counseling and Support: Ongoing therapy and participation in support groups help individuals build coping strategies and maintain their recovery journey.
Should You Use Xanax for Alcohol Withdrawal?
Can Xanax help with alcohol withdrawal? Technically, the answer is yes. Even though Xanax can be helpful in managing specific symptoms of alcohol withdrawal, its use should be carefully considered and monitored due to the potential risks of dependence and abuse. Longer-acting benzodiazepines are typically preferred for their safety and efficacy. Southeastern Recovery Center believes in creating a comprehensive treatment approach, including medical supervision, supportive care, and psychological support. We believe that this is essential for managing alcohol withdrawal effectively and promoting long-term recovery. Reach out to our expertly trained staff to learn more about our alcohol use disorder treatment options.