Understanding Your Coverage Limits and Benefits for Rehab in North Carolina
Navigating the path to recovery from drug and alcohol addiction can be challenging, and understanding insurance coverage for rehabilitation services is a critical part of this journey. In North Carolina the specifics of insurance coverage for drug and alcohol rehab can vary significantly based on the type of insurance plan, the insurer’s policies, and individual circumstances. Southeastern Recovery Center explores how many times insurance will pay for drug and alcohol rehab in North Carolina, helping individuals and families make informed decisions about their treatment options.

In-Patient and Outpatient Treatment and Coverage in North Carolina
In North Carolina, rehabilitation services often include inpatient and outpatient drug and alcohol treatment programs for substance use disorders.
Each type of rehab comes with its own set of coverage details and limitations that vary by insurance provider and policy.
Inpatient Rehabilitation
Inpatient rehab involves staying at a treatment facility for an extended period, providing a structured environment for recovery. In North Carolina, insurance coverage for inpatient rehab typically includes a set number of days per benefit period, which could be a calendar year or a plan year. The number of covered stays per year can vary:
- Private Insurance: Most private insurance plans, including those purchased through the Health Insurance Marketplace, cover inpatient rehab to some extent. The extent of coverage can range from 30 to 90 days per year, and some policies may allow multiple stays within a year if deemed medically necessary.
- Medicaid: North Carolina Medicaid provides coverage for inpatient rehab services, but the specifics depend on the managed care organization (MCO) administering the benefits. Generally, Medicaid covers one inpatient rehab stay per calendar year, with the possibility of additional stays if authorized based on medical necessity.
- Medicare: For those eligible for Medicare, Part A covers inpatient rehab services if hospitalization is required. Coverage typically includes up to 60 days in a rehab facility, with additional stays requiring higher co-pays.
Outpatient Rehabilitation
Outpatient rehab allows individuals to receive treatment while living at home, making it suitable for those with less severe addictions or as a step-down from inpatient care. Insurance coverage for outpatient rehab can include:
- Private Insurance: Outpatient rehab coverage under private insurance often includes a set number of therapy sessions per year. Policies might cover anywhere from 20 to unlimited sessions, depending on the plan. It’s crucial to check if there are caps on the number of covered sessions and whether these caps are annual or lifetime limits.
- Medicaid: North Carolina Medicaid covers outpatient rehab services, usually allowing a certain number of therapy sessions per year. These services are often provided through behavioral health managed care organizations, which may have different limits and authorization requirements.
- Medicare: Medicare Part B covers outpatient rehab services, including counseling and therapy sessions. There are typically limits on the number of covered sessions, and services must be deemed medically necessary.
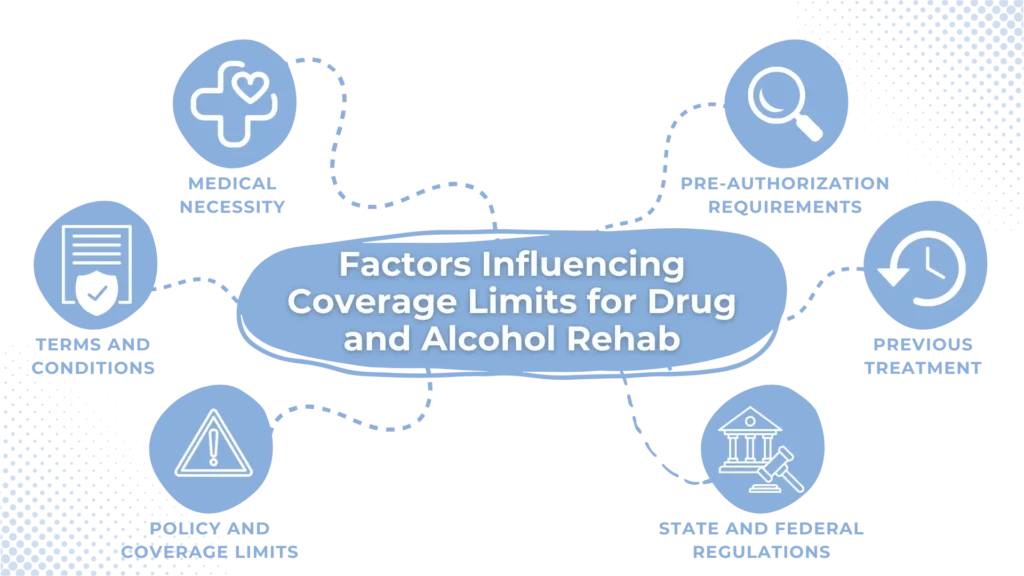
Factors Influencing Coverage Limits for Drug and Alcohol Rehab
Several factors influence how many times insurance will pay for drug and alcohol rehab in North Carolina:
- Medical Necessity: Insurance companies generally require proof of medical necessity to approve rehab services. This proof involves documentation from healthcare providers detailing the patient’s condition, treatment plan, and the need for rehab. Demonstrating medical necessity can often lead to approval for multiple stays or extended coverage.
- Policy Terms and Conditions: Each insurance policy has specific terms and conditions regarding coverage limits. These details include the number of covered days for inpatient rehab, the number of outpatient sessions, co-pays, deductibles, and out-of-pocket maximums. Reviewing the policy terms helps in understanding the extent of coverage and planning treatment accordingly.
- Treatment for Substance Use Disorders in the Same Year: In most instances, your insurance will cover your treatment within the first year with few questions asked. If, within the same year, you request treatment again, you may be required to advocate for yourself or have the rehabilitation center advocate for you. Three or more requests for treatment may require specialized treatment plans to be reviewed because your carrier may think that the rehab isn’t working.
- Length of Treatment for Substance Use Disorders in the Past: If your first round of treatment at a drug and alcohol rehab center was short-lived, insurance may be willing to pay for another round of treatment – for instance, if you did a medical detox and then transitioned to a lower level of care versus a full 90 day program.
- Pre-Authorization Requirements: Many insurance plans require pre-authorization for rehab services. Pre-authorization involves obtaining approval from the insurer before starting treatment. This step ensures that the services will be covered and helps avoid denied claims later. Failing to get pre-authorization can result in out-of-pocket expenses for services that the insurer might otherwise cover.
- Unique Policy and Coverage Limits: Some plans fully cover the first residential treatment stay, but may offer reduced coverage for subsequent treatments. Your attendance history and relapse record are considered when determining coverage. If you have co-occurring mental health conditions, treatment for these may be prioritized, with substance use treatment as a secondary focus.
- State and Federal Regulations: North Carolina follows federal regulations under the Affordable Care Act (ACA), which mandates coverage for substance abuse treatment as an essential health benefit. However, the specifics of coverage, including the number of covered stays and sessions, can vary based on the insurance provider and plan.
Does Insurance Cover Rehab After Relapse?
Many health insurance plans, including those offered through the Affordable Care Act, provide some level of coverage for addiction treatment, recognizing addiction as a medical condition that requires ongoing care. Policies often include coverage for detoxification, inpatient and outpatient rehab, therapy, and aftercare services. Many rehab centers offer assistance in navigating insurance benefits to ensure that patients receive the necessary care for recovery, even after a relapse.

Maximizing Insurance Coverage for Rehab in North Carolina
To maximize insurance benefits for drug and alcohol rehab in North Carolina, consider these six steps:
1. Review Your Insurance Policy
Thoroughly review your insurance policy to understand the coverage limits for rehab services. Pay attention to the sections on substance abuse treatment, including any limitations on the number of covered days or sessions. Knowing these details helps in planning your treatment and avoiding surprises.
2. Verify Coverage with Your Insurer
Contact your insurance provider to verify coverage for rehab services. Ask specific questions about the number of covered days for inpatient rehab, the number of outpatient sessions, and any conditions for coverage. This verification will give you a clearer picture of your benefits and any potential out-of-pocket costs.
3. Obtain Pre-Authorization
Ensure you obtain pre-authorization for rehab services, if required by your plan. This step is crucial to secure coverage and avoid denied claims. Work closely with your healthcare provider to gather the necessary documentation and submit it to your insurer.
4. Work with Healthcare Providers
Collaborate with your healthcare providers to document the medical necessity of rehab services. Detailed documentation can strengthen your case for coverage, especially if multiple stays or extended treatment is needed. Your provider can also help you navigate the insurance requirements and appeal processes if necessary.
5. Appeal Denied Claims
If your insurance claim for rehab services is denied, don’t give up. You have the right to appeal the decision. Gather supporting documentation, including letters from healthcare providers, and submit an appeal to your insurer. Persistence can pay off, and many denied claims are overturned on appeal.
6. Explore Additional Resources
If insurance coverage is insufficient, explore additional resources for funding rehab. North Carolina offers state-funded programs, grants, scholarships, and sliding scale fees based on income. Non-profit organizations and rehab centers may also provide financial assistance or payment plans.
Get Help Navigating Your Insurance Coverage For Rehab in North Carolina
Understanding how many times insurance will pay for drug and alcohol rehab in North Carolina requires a thorough review of your insurance policy and proactive communication with your insurer. Coverage limits vary widely based on the type of rehab, the insurance plan, and the specifics of the policy. If you need help reviewing your policy, Southeastern Recovery Center is here to help. Our experienced staff handles insurance claims and billing daily – with expertise in helping you maximize your private insurance benefits.
If you or a loved one is considering drug and alcohol rehab, contact Southeastern Recovery Center today to learn more about our individualized treatment plans and to get quick insurance verification.