Healthcare professionals are often looked at as heroes and saviors, and in some cases considered larger-than-life. This makes sense: doctors, nurses, and mental health workers help save lives both in the short term and long term. However, medical professionals have their own occupational hazards that can put their lives at risk.
One of these occupational hazards is addiction to drugs or alcohol. Due to the high-stakes environment and social conditions that medical professionals find themselves in, some may turn to drugs to help manage stress symptoms, only to expose themselves to other adverse effects. If anything, this just goes to show how even the most knowledgeable of people can struggle to resist drugs and alcohol and might need help once they’ve developed an addiction.
Article Preview:
Addiction in Healthcare Professionals. Healthcare professionals are just as susceptible to becoming addicted to drugs and alcohol.
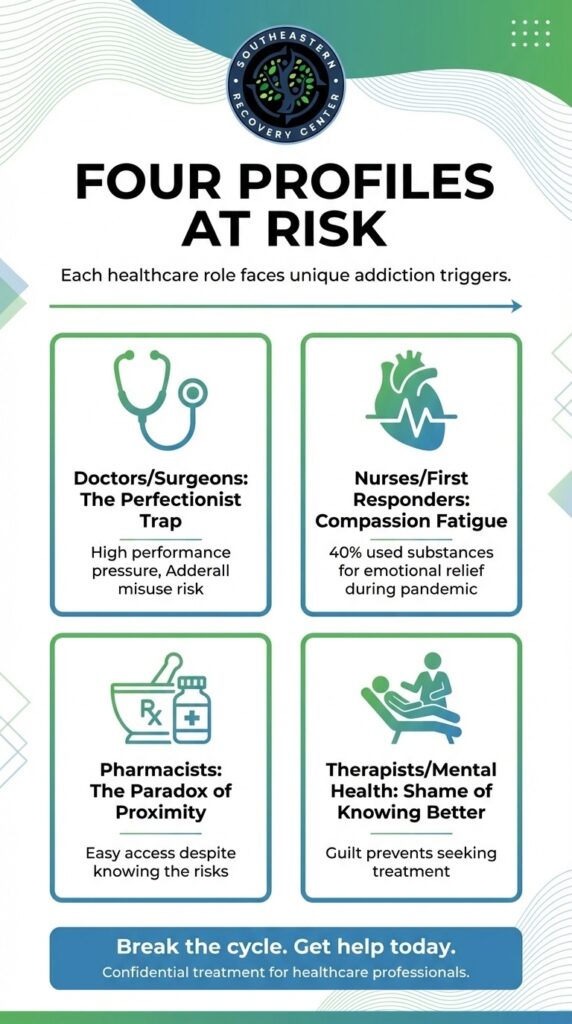
Doctors & Surgeons (The Perfectionist Trap). Doctors and surgeons seek consistent high performance, which can lead them to develop an addiction to drugs like Adderall.
Nurses & First Responders (The Compassion Fatigue Factor). Nurses and first responders are exposed to high stress situations and potent emotions, which lead them to want to self medicate to deal with anxiety.
Pharmacists (The Paradox of Proximity). Pharmacists have extreme ease of access to pharmaceutical drugs, which can lead them to abuse substances.
Therapists & Mental Health Workers (The Shame of Knowing Better). Therapists and mental health workers may shy away from seeking treatment for drug and alcohol addiction, feeling as if they’re expected to know better.
FAQs about Why Addiction is an Occupational Hazard for Healthcare Professionals. Learn frequently asked questions about addiction as it relates to healthcare professionals.
Addiction in Healthcare Professionals
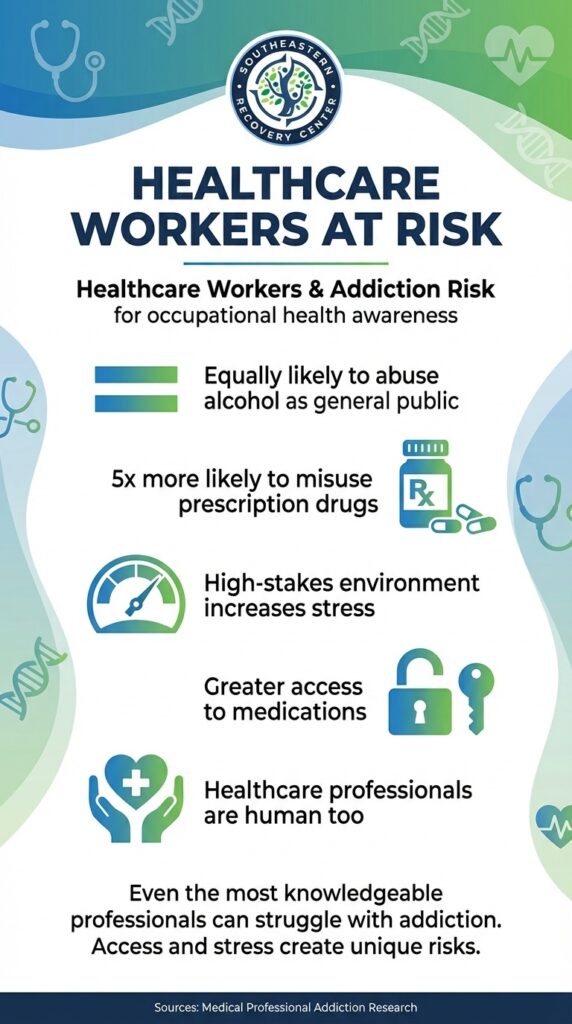
The idea of healthcare professionals succumbing to drug and alcohol addiction might be surprising, but at the end of the day these highly trained individuals are still human. They can turn to drug use for the same reasons that other individuals do: for stress relief, to self medicate for pain, anxiety, or depression, because they want to feel a shot of dopamine or sense of euphoria.
Access is one of the primary factors that fuels drug use and the general population, and doctors and nurses have easier access to drugs than most. Perhaps this is why those physicians are about equally likely that the general public to abuse alcohol or illegal drugs, they’re five times as likely to misuse prescription drugs.
When we look at the common psychological profiles healthcare professionals individually, you can better understand how medical professionals can fall into drug use:
Doctors & Surgeons (The Perfectionist Trap)
Both doctors and surgeons work in fields that are competitive and demand high-performance, day in and day out. Lives are on the line. This fosters an environment where doctors and surgeons may feel pressure to not be held back by natural human feelings such as fatigue or brain fog. A push towards maintaining perfectionism at all times can naturally lead doctors and surgeons to abuse prescription medication such as Adderall, which is known for impacting an individual’s ability to focus.
While doctors and surgeons can take prescription medication, they have to be referred by other medical professionals. They can’t self prescribe. And yet, access to drugs like Adderall might tempt them towards using them illegally, which can then naturally lead into misusing these drugs while chasing perfectionism. In fact, studies have suggested just that, with one such study noting that certain dimensions of perfectionism are positively correlated with illicit use of prescription stimulants.
Nurses & First Responders (The Compassion Fatigue Factor)
Nurses and first responders see to individuals seeking urgent care. This means managing steady stress while on the job while also encountering individuals in extreme situations, whether they’re near death suffering from severe health conditions, to say nothing for the chance of encountering various bodily fluids. Plus, first responders and nurses may be subject to the brunt of emotions from patients and their families and even made out to bear the responsibility of negative health outcomes.
Individuals don’t get into these professions without having a large amount of compassion. And yet, that same compassion may lead them to feel almost as strongly as their patients and their families do when they are exposed to negative emotions. This can result in strong feelings of depression and nurses and first responders, which can then lead to them seeking out self-medication through the use of drugs or alcohol. A study by Florida Atlantic University found that during the pandemic, 40% of first responders admitted to using substances to relieve emotional discomfort.
As we see often in the stories of people visiting Southeastern Recovery Center at our Charlotte, North Carolina location, it’s easy to go from using substances to relieve emotional discomfort to developing a dependence on the substances, which is the first step in developing a substance use disorder.
Pharmacists (The Paradox of Proximity)
Pharmacists deal with daily job stress in the form of needing to get prescriptions right. This means not only matching patients with their intended prescriptions, but also making sure to properly guide their usage of said prescriptions. There’s also the occasional stress of blowback to deal with when a patient can’t afford their prescription.
But really, the primary factor impacting pharmacists developing drug addiction is likely their proximity.
Pharmacists are in a paradox or proximity. At the pharmacy, they are among the individuals that know the most about all the drugs that they deal with, including their proper usage and potential negative side effects. However, they are also individuals that have the most access to a litany of prescription drugs. Pharmacists feeling the pressure of their stressful job, or feeling any other negative emotion that other people feel, such as depression, anxiety, PTSD, may seek to self medicate. It’d certainly be easy enough for them to.
Even though pharmacists are aware of the potential risks of developing a dependence or addiction to drugs, people often underestimate just how difficult it can be to defeat a drug addiction once it has begun requiring your brain chemistry and bodily functions. When seizing intake of a drug might lead to withdrawal symptoms, it’s easy to understand how pharmacists might self medicate and quickly find themselves trapped in a loop of drug usage.
Therapists & Mental Health Workers (The Shame of Knowing Better)
Therapists and mental health workers might also find themselves falling into drug addiction. Stress, anxiety, depression, and more all mental health disorders that can lead even these healthcare professionals into attempting to self medicate, which can lead into developing a substance use disorder.
But the real kicker for therapists and mental health workers is that they might not be able to bring themselves to check into a rehab facility like Southeastern Recovery Center.
The shame of knowing better, as in, the belief that some therapist mental health workers hold that they should know better than to have developed drug addiction in the first place, might prevent them from seeking out help. Instead, they’ll continue to suffer the adverse life impacts of drug addiction, all the while understanding how harmful they are yet not being able to get out of the mental trap.
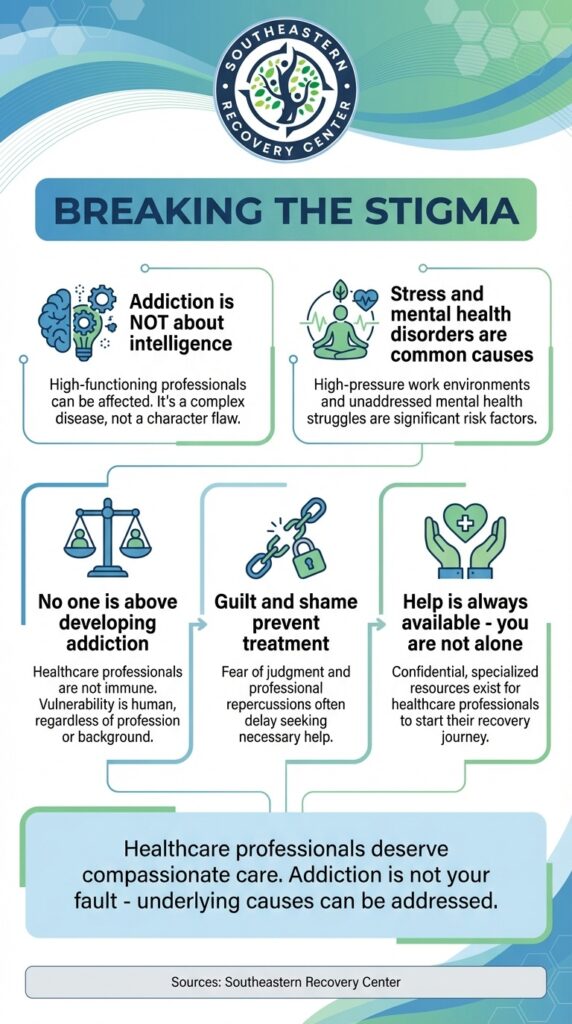
Guilt and shame are powerful emotions that keep individuals from seeking treatment for their drug or alcohol addiction. That’s why we focus on helping individuals understand that addiction is not their fault. Instead, we prefer to address the underlying causes that lead an individual to develop drug and alcohol dependence or addiction in the first place.
At the end of the day, no one, not even healthcare professionals, are “above” developing drug and alcohol addiction. The belief that they are is a false one, and a harmful one, that prevents individuals from being able to receive the care that they need the moment that they need. Instead, we should foster understanding of how powerful addiction can be, as well as spread the knowledge that no matter how severe addiction seems, help is always available.
FAQs about Why Addiction is an Occupational Hazard for Healthcare Professionals
Are healthcare professionals as likely to get addicted to drugs as regular people?
Yes, healthcare professionals are just as likely to get addicted to drugs as regular people.
What kind of drugs do healthcare professionals get addicted to?
Two common drugs that healthcare professionals get addicted to include oxycodone and fentanyl.
Aren’t healthcare professionals too smart to get addicted to drugs?
No, healthcare professionals aren’t too smart to get addicted to drugs, nor is drug addiction a matter of intelligence. Healthcare professionals work stressful jobs, and being under stress experiencing mental health disorders such as anxiety are common causes that lead individuals to seek out drugs for self-medication.
Do healthcare professionals have more access to drugs than regular people?
Yes, healthcare professionals have more access to drugs and regular people, which means they have more temptation and ease when it comes to trying out addictive drugs such as fentanyl and opioids.
Sources:
https://gme.med.ufl.edu/files/2014/02/Drug-Abuse-Among-Doctors.pdf
https://files.eric.ed.gov/fulltext/EJ1222138.pdf
https://www.fau.edu/newsdesk/articles/first-responders-pandemic-study.php